Navigating Postpartum Depression: 5 PPD Tips
5 Essential PPD Tips for Women of Color: Navigating Postpartum Depression with Support and Education
Dear Mama,
You are not alone. Even it when it feels like you are.
By now, we’ve all either heard the term postpartum depression, experienced it for ourselves, or witnessed it in a friend or loved one. No matter how much we understand it in theory, the experience can be jarring and unrecognizable. In communities of color, postpartum depression can sometimes be misunderstood, misdiagnosed, or mistreated by medical professionals. This is due to many assumptions that are placed on the experience of motherhood, embedded cultural belief systems, racial discrimination in healthcare settings, or not having enough time to tune into ourselves and notice. For women of color, our symptoms can be dismissed or minimized by friends, family, community, or medical providers, leaving many to feel isolated or alone in their experiences. Finding PPD tips that address the unique challenges faced by women of color can provide support and validation during this difficult time.
Stats
Women of color are 25% more likely to experience postpartum depression but are 50% less likely to seek treatment. Many limiting factors contribute to this including limited access to competent care, an even more limited number of mental health providers that are trained in perinatal mental health, lack of screening and treatment support during postpartum visits etc. Women of color are less likely to be screened and diagnosed with a perinatal mood and anxiety disorder or PMAD than White women. Over the past few years, many organizations have made extenuating efforts to close the gap in care and educate communities of color on the signs and risks of postpartum depression. Still, the data indicates that there's so much more to be done.
There are also cultural factors that contribute to limited diagnosis and treatment for postpartum depression, including:
Mental health stigma
General misinformation
Lack of culturally competent providers
Spiritual bypass (the tendency to use spiritual beliefs or practices to avoid facing unresolved emotional issues)
This isn't to demonize or blame anyone or any culture, most support for moms is generally well intended but many of our mothers and grandmothers didn’t have the time, energy, or language to describe postpartum depression or better understand it. Not to mention that postpartum depression is more prevalent now than ever, now that we are living in communities that are less connected with a larger community, more women work outside the home, and the cost of childcare is astronomical.
Education
Now, let’s cover the basics… What is postpartum depression?
Postpartum depression is an overwhelming sense of hopelessness that occurs post-delivery between 2-6 weeks after birth. Symptoms of postpartum depression include:
Sleep disturbances
Consistent and unshakable low mood
Irritability or Anger
Lack of ability to care for oneself or the baby
Lack of appetite
Why is screening so important?
Early screening of postpartum depression has been statistically proven to yield better outcomes for recovery, treatment, and early bonding with an infant. Currently, most women will only receive a screening from an OBGYN at the 6-week postpartum visit, but nothing else. There is a lot of advocacy towards increasing the frequency of this, but most women will only receive one screening during the postpartum period.
5 Tips for coping with postpartum depression as a woman of color
Step 1. Undoing internalized cultural beliefs about depression.
You may have thoughts swirling around that are minimizing or trying to disprove your depression. “Oh, it’s just baby blues” or “You just need to get outside, you’ll be okay”, or “Being a mom is hard, it’ll get better soon”. These thoughts are natural, but often not supportive of our mental health. The difference between baby blues and depression is duration and intensity. Baby blues typically subsides within two weeks and is due to the natural fluctuation of hormones post-birth. Depression, on the other hand, will persist past the two weeks and limits our ability to care for ourselves and/or our little one.
So let’s start by noticing if our mind is filled with internalized beliefs from society, our family, or our culture that are not supportive. This is where you get to discern whether or not these thoughts are useful or not.
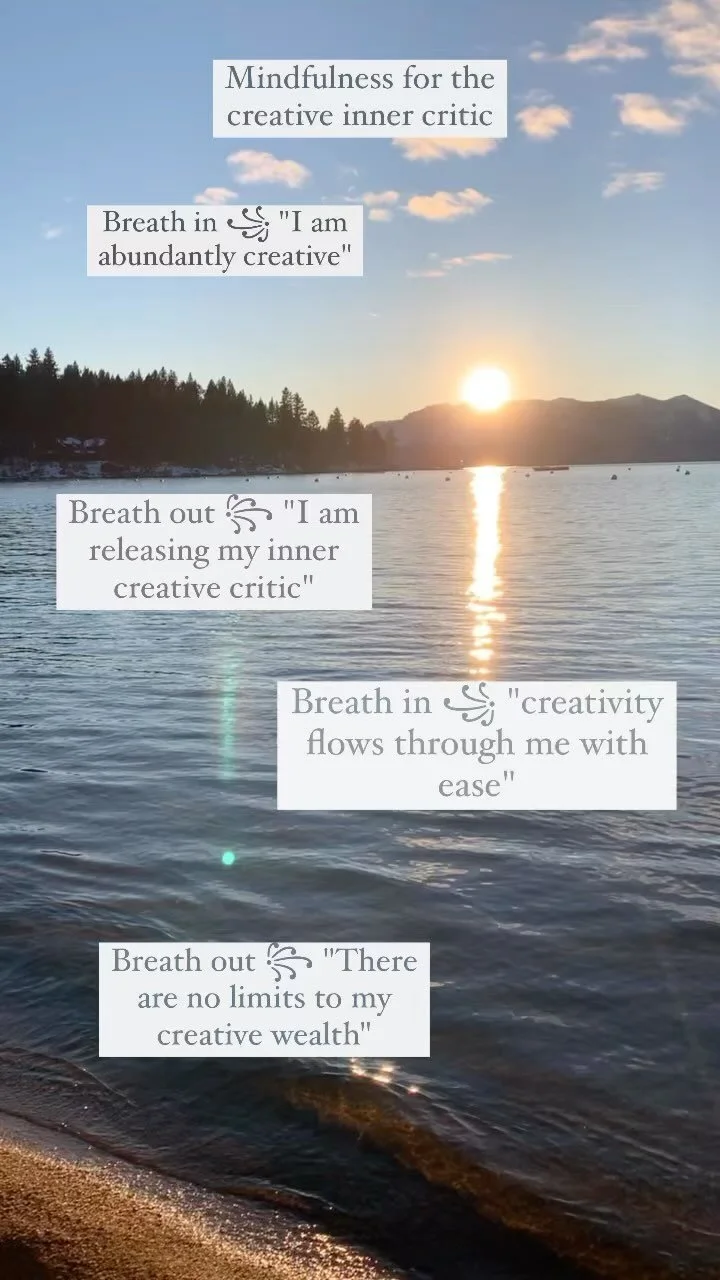
The RAIN method by Tara Brach is an effective tool for assessing our thoughts or emotions. It stands for:
Recognize what is going on
Allow the experience to be there; just as it is
Investigate with interest and care
Nurture with Self-Compassion
Step 2. Support. Support. Support.
It has been researched and proven that a support network is one of the best supportive mechanisms for postpartum depression. But in today’s society, many parents live far from loved ones, may not have strong peer support, or struggle to make and build community. Others may have support nearby but struggle to ask for help or feel neglected and isolated from the community. If you do not have a built-in community of peers, family, or community, we have to get creative. Here are a few suggestions on where to start building a community:
Facebook groups for mothers in your neighborhood
Local WhatsApp groups for your neighborhood - I randomly found out about one in my neighborhood while bumping into a mom at the playground
PSI support groups - all on Zoom and have specific cultural groups as well.
Spiritual or religious groups
If you have a support group but struggle to ask for support, assess the barriers to asking for support. Do you assume everyone is busy? Do you not want to be a “burden to others”? Then ask yourself are these thoughts 100% factual or based on feeling? If they are feelings-based, then it’s worth doing some reality testing. It also helps to get specific about how people can support you. Would you like for someone to just hold the baby so you can nap? Do you need help with laundry? Do you need someone to watch funny movies with you? Do you need a pediatric referral for your colicky baby?
For example, I assumed many of my peer friends would be too busy to support with meals when I was postpartum. When my daughter entered the NICU a friend asked how they could support. Instead of saying “oh I’m okay don’t worry about it”, I got REALLY specific. “Actually, could you put together a meal train and send it to our friends?” Low and behold people signed up to drop off meals over the next two weeks and if they couldn’t, they either declined or offered support in another way. This is an ideal example of course, but we never know how much our community is willing to support if we don’t ask. It takes risk taking, but it’s worth a shot.
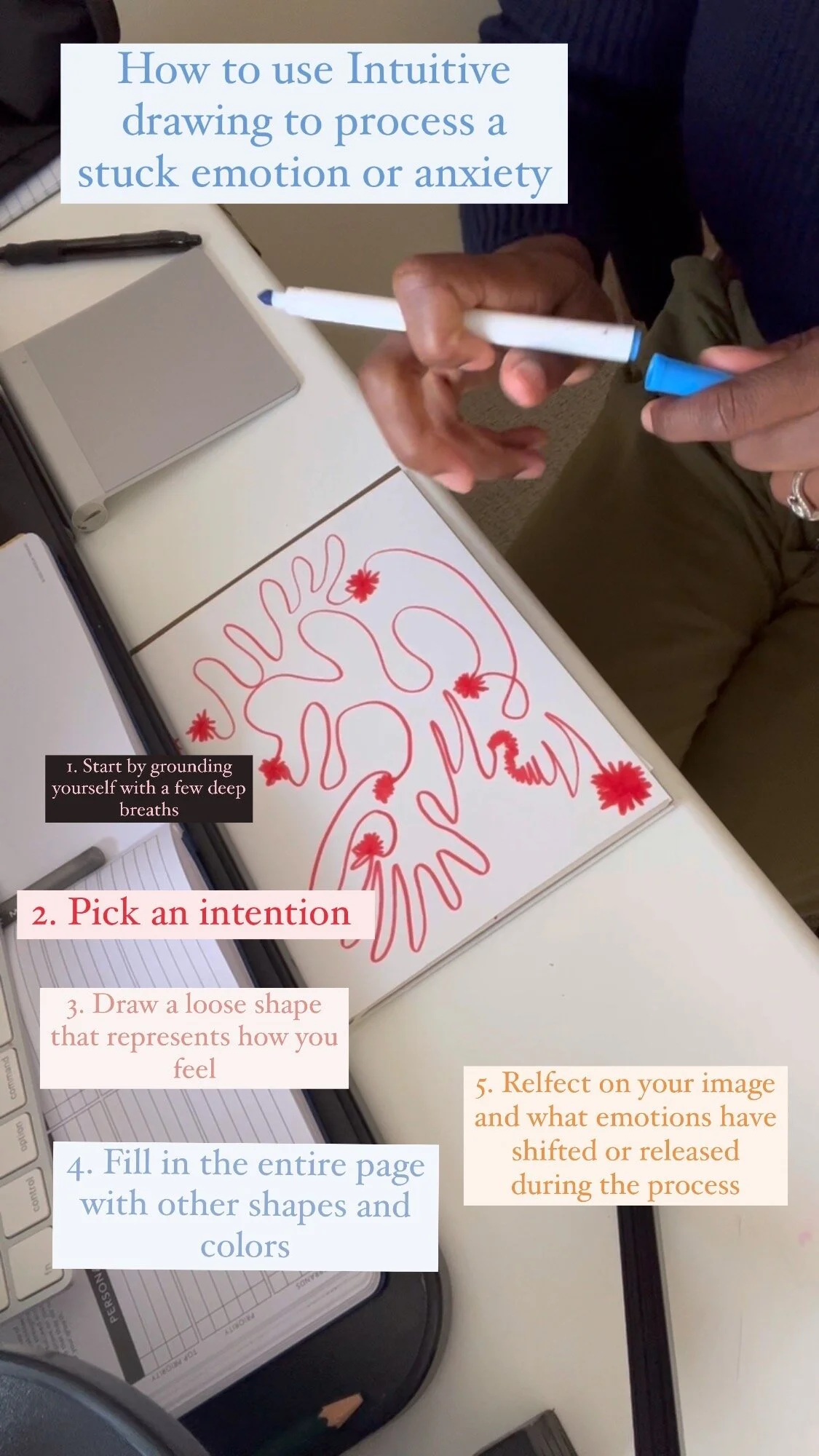
Step 3. Body assessment.
Assess your needs. Especially food intake and movement. Check-in with how much you have been able to eat and move throughout the day. If you have a low appetite grab some nutrient-dense bars or fruit and have those throughout the day. Something is better than nothing when it comes to nourishment. Try getting more sunlight even if it means just opening windows to receive more sun. The more vitamin D the better. Think of movement and nourishment as your body’s baseline needs for functioning. This is a starting point. It doesn’t have to be perfect and it’s not going to magically cure your PPD, but it will give your body a place to start in treating your postpartum depression.
Step 4. Seek professional support and Advocate for your needs
If possible, seek support from a professional immediately. A licensed mental health professional will not only provide empathy and support during this crucial moment in parenthood, but also recommend specific tasks and tools to enact change and get you closer to the parent you want to be. I recommend the Postpartum Support International directory because all practitioners listed are certified in perinatal mental health (like me). If cost is a barrier I recommend checking out my list of affordable mental health resources or looking into using out of network benefits.
You can also visit your primary care physician or OBGYN and ask for mental health referrals, many medical offices will have referrals available. I would also recommend asking to take the postpartum screening again to assess for postpartum depression if you are unsure.
If you are feeling unsafe to yourself or others, that is a sign to seek help at your nearest hospital as soon as possible.
5. Medication support.
I know there is a ton of stigma around taking medication for your mental health, but some medications have been proven to be effective and safe for postpartum use. I often tell clients that the decision is ultimately their own, but it’s worth consulting with a psychiatrist about. The more information we have, the more empowered we are to make the best decision for ourselves. Because so many doctors are not specifically trained in perinatal mental health it’s beneficial to use a directory like the one Postpartum Support International to find a practitioner that is most knowledgeable about medication use that is safe during postpartum.
Additional Resources
PSI - Postpartum Support International - Educational Resources and Support Groups
To seek immediate help or support:
Postpartum Support International (PSI) Helpline
Phone: 1-800-944-4773
Website: Postpartum Support International
Offers support and resources for postpartum depression and anxiety.
National Suicide Prevention Lifeline
Phone: 1-800-273-TALK (1-800-273-8255)
Website: National Suicide Prevention Lifeline
Provides 24/7, free, and confidential support for individuals in distress.
The National Motherhood Helpline
1-800-994-6600
In conclusion, postpartum depression is a significant challenge that affects many women, especially those from diverse backgrounds. Understanding the unique experiences and disparities faced by women of color is crucial in addressing this critical issue. By seeking professional help, building a supportive network, and prioritizing self-care, mothers can find pathways to healing and recovery. Remember, you are not alone in this journey—reaching out for support is a sign of strength, not weakness. By fostering awareness and promoting access to resources, we can work together to create a supportive environment for all mothers, ensuring that everyone has the opportunity to thrive during this transformative period of life.
If you’re a mother residing in California and are feeling overwhelmed, anxious, or experiencing symptoms of postpartum depression, you don’t have to go through it alone. I offer compassionate, culturally competent therapy services designed to support you through this challenging time. Reach out today to learn more about how therapy can help you regain balance and find healing. Your well-being matters, and taking the first step toward professional support is an act of strength. Contact me for a free consultation, and let’s work together on your journey to wellness.